World Malaria Day 2025: reinvest, reimagine and reignite our commitment to end malaria
On this World Malaria Day, we reflect on the theme ‘Malaria Ends with Us: Reinvest, Reimagine, Reignite.’ This theme serves as a reminder that over 90% of malaria cases and deaths occur in Africa, where pregnant women, infants, and children are disproportionately affected. EDCTP reaffirms its commitment to supporting the development of innovative medical interventions for the diagnosis, prevention, and treatment of malaria. Furthermore, product-focused implementation research is crucial to ensure that these interventions reach those who need them most. Recent findings from EDCTP-supported studies offer new hope in the quest for malaria eradication.
Investing in malaria research
The advancement of research and development (R&D) for new and improved tools is vital in the fight against malaria. Through its strategic business plan, EDCTP2 has supported research that evaluates new drugs and drug combinations, particularly for children and pregnant women suffering from malaria. Given that many individuals living with HIV reside in malaria-endemic regions, it is essential to understand the interactions between antimalarial drugs and antiretroviral therapies (ARVs). EDCTP2 also supports strategies to enhance access to drugs, vaccines, and diagnostics, as well as malaria elimination initiatives.
Additionally, EDCTP actively supports activities in sub-Saharan Africa that foster an environment for conducting innovative research addressing the challenges posed by malaria, including strengthening the role of community engagement in the existing local health systems.
Between 2014 and 2025, EDCTP2 invested €157.2 million to support 65 projects on malaria research, from collaborative clinical studies implemented by African-European research consortia to projects conducted by EDCTP Fellows leading the malaria research agenda in Africa.
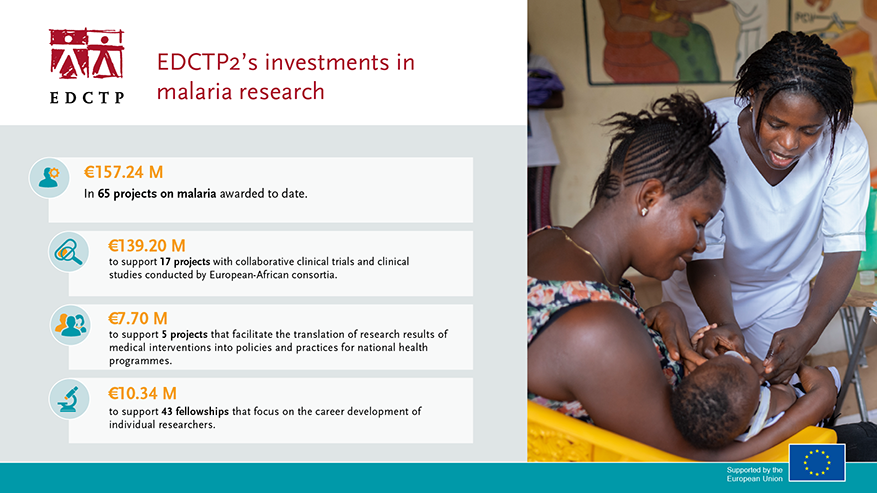
Since 2021, Global Health EDCTP3 has committed €43.3 million to 11 collaborative research projects on malaria, building on the success of the previous EDCTP programmes. Under its Work Programme 2025, Global Health EDCTP3 has launched a call for proposals aimed at research on existing malaria therapeutics and clinical development of new antimalarial candidates, with an indicative budget of €30.9 million.
Supporting innovative medical interventions against malaria
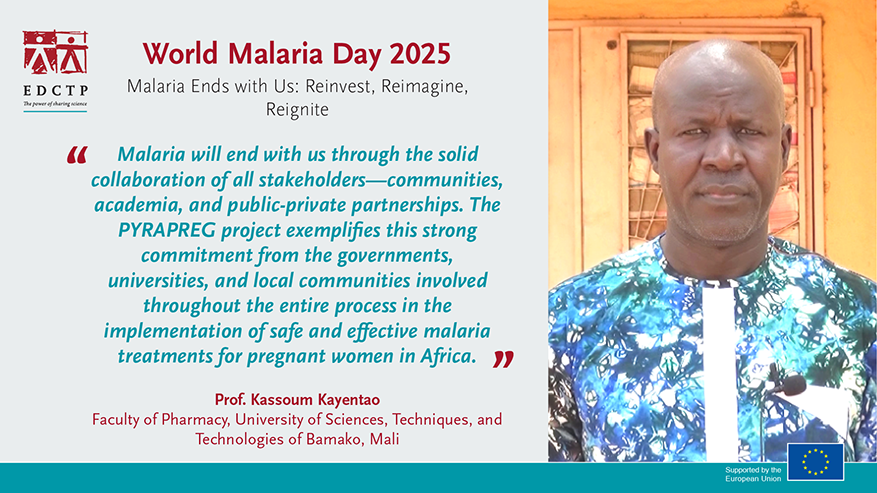
Malaria in pregnancy can be harmful to both mother and child, causing maternal anaemia and low birth weight. Several artemisinin-based combination therapies are recommended for the treatment of malaria in the second and third trimesters of pregnancy, but they vary in their efficacy, safety and tolerability. The PYRAPREG study implemented a large-scale trial to evaluate pyronaridine-artesunate – Pyramax®(PA) use in pregnant women with uncomplicated falciparum malaria. The study was implemented in 5 African countries (Burkina Faso, The Gambia, Democratic Republic of Congo, Mali and Mozambique), with the collaboration of institutions in the Netherlands, Spain and the United Kingdom. Preliminary results have indicated that PA is safe and efficacious for the treatment of malaria in the second and third trimesters of pregnancy, indicating that PA could be the next ACT to be used for the management of malaria in pregnancy. Final results for the primary endpoints are expected to be available later in 2025.
Re-investing in proven therapies
and increases the risk of birth complications. One approach known to be effective, and recommended by WHO, is the preventive use of antimalarial drugs, known as ‘Intermittent Preventive Treatment of malaria in Pregnancy’ (IPTp), which can be integrated into antenatal care. However, in countries such as Kenya, only 25% of pregnant women receive three or more doses of IPTp. To address this gap, the Revive IPTp project is working with communities, health workers and health authorities at a devolved level in Kenya to reinvigorate malaria control in pregnant women.
The project aims to close the gap with the national target of 80% coverage of IPTp-SP for pregnant women by the end of 2025. Findings published in the Malaria J. in 2023 and Frontiers in Global Women’s Health in 2024, showed there is an imperative need for health literacy programmes that focus on increasing knowledge of IPTp-SP dosage, timing and benefits for both the young pregnant mother and her foetus. Community engagement through dialogue with mentor mothers and male partners will be an important complementary approach in establishing a support system for young women for positive health outcomes, including attaining the recommended 3+ doses of IPTp-SP prophylaxis.

Another proven strategy that is not fully implemented is Seasonal Malaria Chemoprevention (SMC). In regions where malaria is highly seasonal, the preventive drug treatment of children during high-risk periods can directly protect them and also reduce the reservoir of parasites capable of causing the disease. Although recommended by WHO, only 50% of eligible children had access to SMC in 2017. Collaborating closely with National Malaria Control Programmes in 13 countries in West and Central Africa, and with support from WHO, the OPT-SMC project aims to expand and enhance the implementation of SMC in sub-Saharan Africa. If high levels of SMC coverage can be consistently achieved across all countries and all regions within countries that have SMC programmes, this may lead to a significant reduction in childhood deaths from malaria.
Preventing malaria in children
Intermittent Preventive Treatment of malaria in Infants (IPTi) with sulfadoxine-pyrimethamine (SP) is recommended by the WHO but has been implemented only in Sierra Leone. With IPTi, a full course of antimalarial drugs is provided to children under 2 years of age at times when they receive routine vaccinations.
The MULTIPLY project aims to increase the uptake of IPTi in Sierra Leone, where only around a third of eligible infants receive the recommended three doses by 9 months of age, and to introduce IPTi in two additional countries, Mozambique and Togo.
The implementation of IPTi began in 2022 and has enrolled around 45,000 children across the three countries, with each country enrolling 15,000 participants. These infants are set to receive up to six doses of IPTi over a two-year period. Interim findings published in the Malaria J. in 2023 indicate a notable increase in coverage, with 50% of children in Sierra Leone receiving the three recommended doses. Despite these advances, further efforts are needed to enhance IPTi coverage, particularly as the strategy expands into the second year of a child’s life, following recent WHO guidelines. The final results from the study in Sierra Leone will be presented in Freetown on 29 April 2025 to the Ministry of Health as well as to other key stakeholders, including national health actors and international organisations such as WHO and UNICEF. It is expected that the enhanced implementation strategy will be scaled up to encompass additional regions and countries with moderate-to-high malaria transmission rates.
Malaria is also a common cause of severe anaemia in children. As well as being associated with significant in-hospital mortality, children remain at risk after discharge. Recent studies show that three months of post-discharge malaria chemoprevention with dihydroartemisinin-piperaquine reduces deaths by 35% and hospital readmissions by six months, though it does not affect non-malarial readmissions. The PDMC-II study combines this treatment with azithromycin to evaluate whether this prophylactic approach can be a cost-effective strategy for managing severe anaemia in malaria-endemic regions, ultimately reducing non-malarial readmissions. Conducted across Kenya, Malawi, and Uganda, with collaborations involving institutions from the Netherlands, Norway, and the United Kingdom, the study is set to follow nearly 1,000 children for 26 weeks post-enrolment.
The study is coordinated by Prof. Kamija Phiri from the Training Research Unit of Excellence in Malawi. Prof. Kamija, a former EDCTP Fellow, was awarded the EDCTP Scientific Leadership Prize in 2023.
Building African scientific leadership against malaria
EDCTP has made significant investments in research capacity through its extensive fellowship programme. Many EDCTP Fellows have assumed leadership positions in African science, generating high-quality research outputs on poverty-related infectious diseases, including malaria. A total of 43 EDCTP Fellows are conducting malaria research.
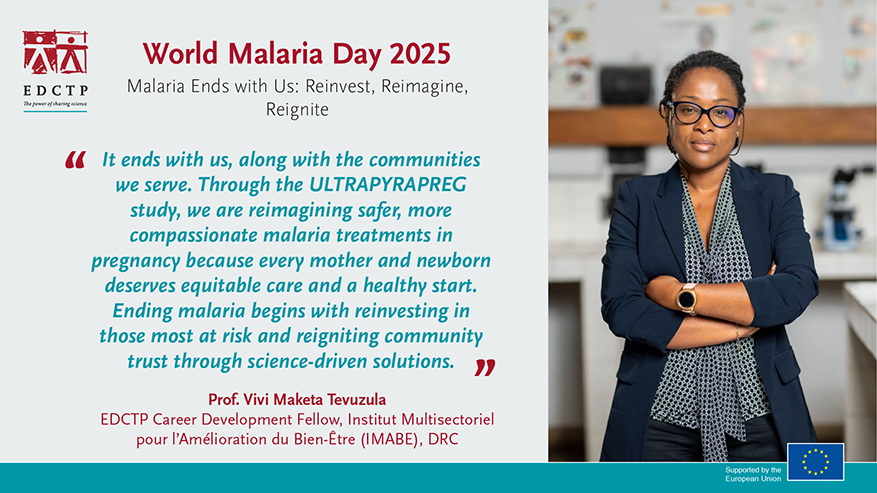
In her EDCTP Career Development Fellowship, Professor Vivi Maketa is assessing whether highly sensitive rapid diagnostic tests for malaria parasites can be used by pregnant women who would benefit from antimalarial treatment during pregnancy.
In a trial in Kinshasa, the Democratic Republic of Congo, she is comparing pregnancy outcomes in women following the standard IPTp approach with sulfadoxine–pyrimethamine with an ISTp strategy incorporating ultrasensitive rapid diagnostic tests followed by treatment with the antimalarial, pyronaridine–artesunate (Pyramax®, PA) as part of the main PYRAPREG study.