World AIDS Day 2023: 20 years of supporting innovative approaches to fight HIV/AIDS
Since its inception in 2003, EDCTP has had a strong focus on one of sub-Saharan Africa’s greatest health challenges: HIV/AIDS. On World AIDS Day 2023, EDCTP joins partners around the globe to support communities – especially those living with HIV – to lead the way to ending HIV/AIDS. This is also an opportunity to look back and reflect on the impact of the clinical research on HIV and HIV-associated infections EDCTP has supported over the last 20 years of the programme.
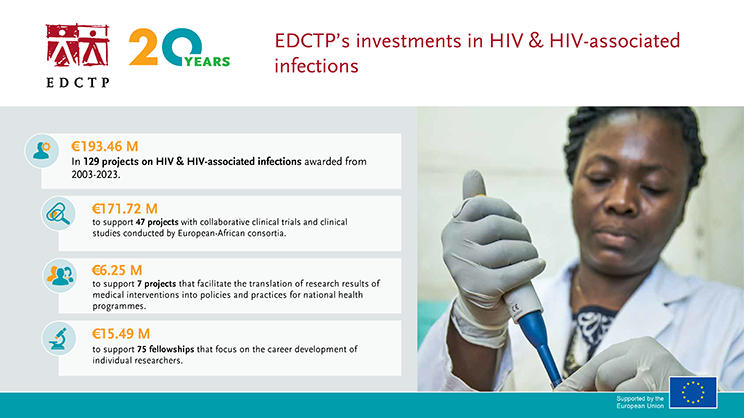
20 years of investments in HIV and HIV-associated infections
Impact on HIV and HIV-associated infections
Clinical research supported by EDCTP addresses the diagnosis, treatment, and prevention of poverty-related diseases such as HIV/AIDs, including how to implement new interventions in the community. We focus on populations often excluded from clinical studies but with major unmet medical needs – including pregnant women, newborns, children, other vulnerable populations, and people with co-infections and comorbidities.
For almost two decades, the CHAPAS Consortium has been conducting clinical trials to improve treatment options for children living with HIV in sub-Saharan Africa. Data from EDCTP-funded CHAPAS–1 and CHAPAS–3 projects supported licensing applications for child-friendly formulations and provided evidence in support of WHO recommendations on updated treatment options. Data from the CHAPAS trials contributed to the approval of fixed-dose antiretroviral drug formulations for children by the US Food and Drug Administration, paving the way for their distribution through global philanthropic programmes and greatly enhancing African children’s access to life-saving antiretroviral drugs. The results of the CHAPAS–4 study, designed to identify an optimal second-line treatment for children with HIV were presented at the International AIDS Society Conference in summer 2023. The trial found that newer antiretroviral combinations including tenofovir alafenamide and dolutegravir were superior to older second-line options for children living with HIV.
There were 1.2 million pregnant women with HIV recorded globally in 2022, with Africa having the highest burden. EDCTP supports research to optimize antiretroviral treatment in pregnant and lactating women to prevent mother-to-child transmission of HIV. The Kesho Bora study – ‘A better future’ in Swahili – provided some of the earliest and strongest evidence that triple antiretroviral therapy could dramatically reduce mother-to-child transmission of HIV during breastfeeding. The findings of the Kesho Bora study, published in 2011, have strongly influenced the revised WHO guidelines on the prevention of mother-to-child transmission of HIV, and infant feeding.
Building on the Kesho Bora study, the PROMISE Consortium has been evaluating how to prevent mother-to-child transmission of HIV during breastfeeding. The PROMISE-PEP study presented results in 2014, showing that two antiretroviral regimens in infants were equally effective in reducing mother-to-child transmission to 1.4% at 12 months, the lowest rate ever reported during breastfeeding. The follow-up study, the PROMISE-EPI study, is testing how interventions to protect infants born to mothers living with HIV can be implemented in the health system. The study is generating real-life data on how effective the prevention of mother-to-child transmission of HIV is; making sure that infants of mothers with high viral load have early access to antiretrovirals at their first vaccination visit; evaluating whether HIV transmission through breastfeeding can be prevented with a simple, single post-natal prophylaxis in infants. PROMISE-EPI has completed follow-ups of more than 34,000 mothers and their babies and reported its results at CROI 2023 showing that the intervention was safe and reduced HIV transmission. The PROMISE-ZERO project, funded by the Global Health EDCTP3 programme is evaluating the intervention in rural and urban areas in Zambia to measure the reduction in HIV transmission and to determine acceptability and barriers to uptake.
HIV prevention strategies that have proven effective in other populations are not working well in adolescents (young people aged 10-24 years), and alternatives are required. The EDCTP-funded CHAPS study has carried out a mix of consultative research to explore attitudes to PrEP among adolescents and young adults, as well as laboratory studies to establish suitable doses of a new drug, tenofovir alafenamide (TAF), for use in PrEP, which has several advantages over the antiretroviral typically used in PrEP, tenofovir. The CHAPS study found that ‘on-demand’ PrEP – taking antiretrovirals when needed rather than daily – was favoured over daily PrEP. Data from the CHAPS trial suggest that on-demand PrEP could be simplified to a double dose of F/TDF or F/TAF given 5–21 h prior to intercourse. The BREATHER-plus trial is testing whether young adults living with HIV in Africa can take weekends off from HIV treatment without impact on suppression of the virus.
To provide women with an improved option for PrEP, the CAPRISA 018 study is evaluating an innovative sustained-release antiretroviral implant. A new implant is being developed incorporating TAF, a highly potent antiretroviral with fewer unwanted side effects than earlier drugs. As sub-dermal implants are already widely available through family planning service in several sub-Saharan African countries, implementation could be relatively straightforward.
TB-IRIS – an excessive immune response against M. tuberculosis – is a common complication in patients treated for HIV-TB co-infection. In 2018, the PredART trial provided the first evidence of an effective strategy to reduce the risk of a potentially fatal complication seen when HIV-infected patients being treated for TB begin antiretroviral therapy. A moderate dose of prednisone given over four weeks to patients with HIV-TB co-infection most at risk of developing TB IRIS, reduced their risk by 30%. The results have already influenced national and international guidelines for managing HIV-TB co-infection.
More information
- WHO World AIDS Day 2023
- EDCTP portfolio on HIV and HIV-associated infections
- UNAIDS World AIDS Day report 2023 ‘Let communities lead’ (PDF)
